
New research posted to the medRxiv* preprint server suggests the Omicron variant produces less severe COVID-19 symptoms than earlier severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) variants.
There was a 74% reduced risk of ICU admission, a 91% reduced risk of death, and no patients with Omicron infections needed mechanical ventilation. In addition, patients infected with Omicron recovered faster and were discharged sooner than patients with Delta infections.
While Omicron may be less severe than other variants, the surge in COVID-19 cases is devastating hospitals and causing severe burnout in frontline workers. An overload of COVID-19 hospitalization may lead to delays in medical care and potentially preventable deaths. The research team advises practicing multiple COVID strategies — wearing masks, isolating when infected, and getting vaccinated — to limit community transmission of Omicron and relieve an overwhelmed healthcare system.

Study: Clinical outcomes among patients infected with Omicron (B.1.1.529) SARS-CoV-2 variant in southern California. Image Credit: anushkaniroshan/Shutterstock
Increasing rate of Omicron infections in late 2021
The researchers collected and analyzed data on positive COVID-19 cases in the Kaiser Permanente Southern California Healthcare system from November 30, 2021, to January 1, 2022.
A total of 88,576 positive COVID-19 cases were reported in outpatients from November 30, 2021, to January 1, 2022. In hospitalized patients, about 26.6% tested positive.
People with Omicron cases were more likely to be in their 20’s or 30’s than Delta cases. Additionally, Delta infections mostly came from lower-income neighborhoods, people who identify as white, and a high risk of comorbidities.
Omicron cases made up 75.5% of COVID-19 cases, including another 51.4% that tested in inpatients settings.
Trend-wise, the number of COVID-19 cases related to Omicron increased weekly. The only exception was the week of Christmas, in which the holiday break lagged the processing of tests.
Analyses showed that repeated infections were more likely with Omicron than Delta. People who had a COVID-19 infection 90 or more days since their current infection were 4.45-fold higher among Omicron cases than Delta cases. Moreover, vaccinated people were more likely to get infected with Omicron than with Delta.
When the researchers collected samples from 1,477 infected patients for sequencing, 100% of SARS-CoV-2 isolates detected through S gene target failure belonged to Omicron.
Of the 288,534 people who were outpatients and followed up and later tested positive, 88 were infected with Omicron and required hospitalization. There were 189 hospitalizations for Delta-related infections.
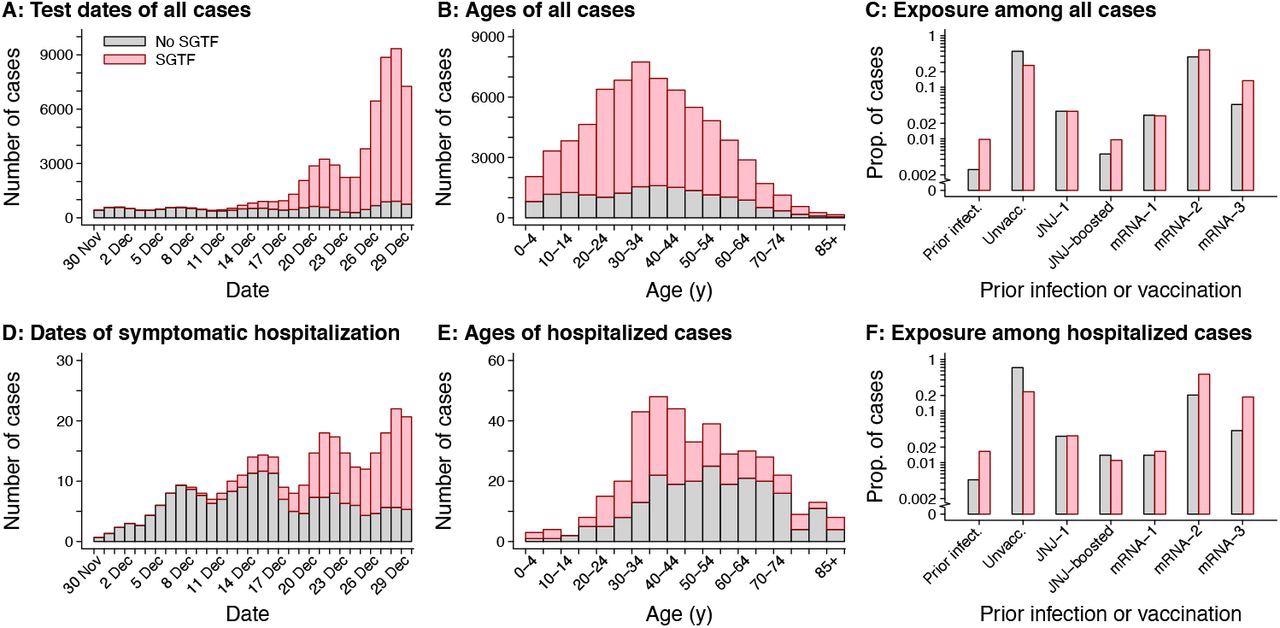
Attributes of cases with SGTF and non-SGTF samples detected. Panels include (A) test dates for all cases analyzed (truncated at 29 December 2022 to accommodate ±1 day jittering); (B) age distribution of all cases analyzed; (C) exposure history (prior documented infection and vaccination) among all cases analyzed; (D) dates of symptomatic hospital admission (truncated at 29 December 2022 to accommodate ±1 day jittering); (E) age distribution of cases with symptomatic hospitalizations; and (F) exposure history (prior documented infection and vaccination) among cases with symptomatic hospitalizations. Pink and grey bars correspond to detections with and without SGTF (interpreted as a proxy for SARS-CoV-2 Omicron variant infection; Table S1), respectively. Totals correspond to samples processed on RT-PCR TaqPath COVID-19 High-Throughput Combo Kit and do not reflect all cases at KPSC.
Severity of disease in hospitalized patients infected with Omicron versus Delta
Out of the 88 admitted Omicron-infected patients, 95.5% presented with symptoms. Similarly, 98.9% of Delta-infected patients were admitted with symptomatic infection.
About 7 patients infected with the Omicron variant required intensive care, including five who were first identified in outpatient settings. One person died. None received mechanical ventilation.
Compared to people admitted with infections from the Delta variant, 23 were admitted to the ICU, 14 patients died, and 11 patients required ventilation.
The daily risk of needing mechanical ventilation was significantly higher among patients with Delta infections than patients with Omicron infections.
About 79.7% of Omicron infections reported acute respiratory symptoms before hospitalization compared to the 80% reported with Delta infections. Once hospitalized, approximately 9.4% of Omicron cases developed respiratory problems. Almost 16% of Delta infections developed respiratory symptoms upon hospitalization.
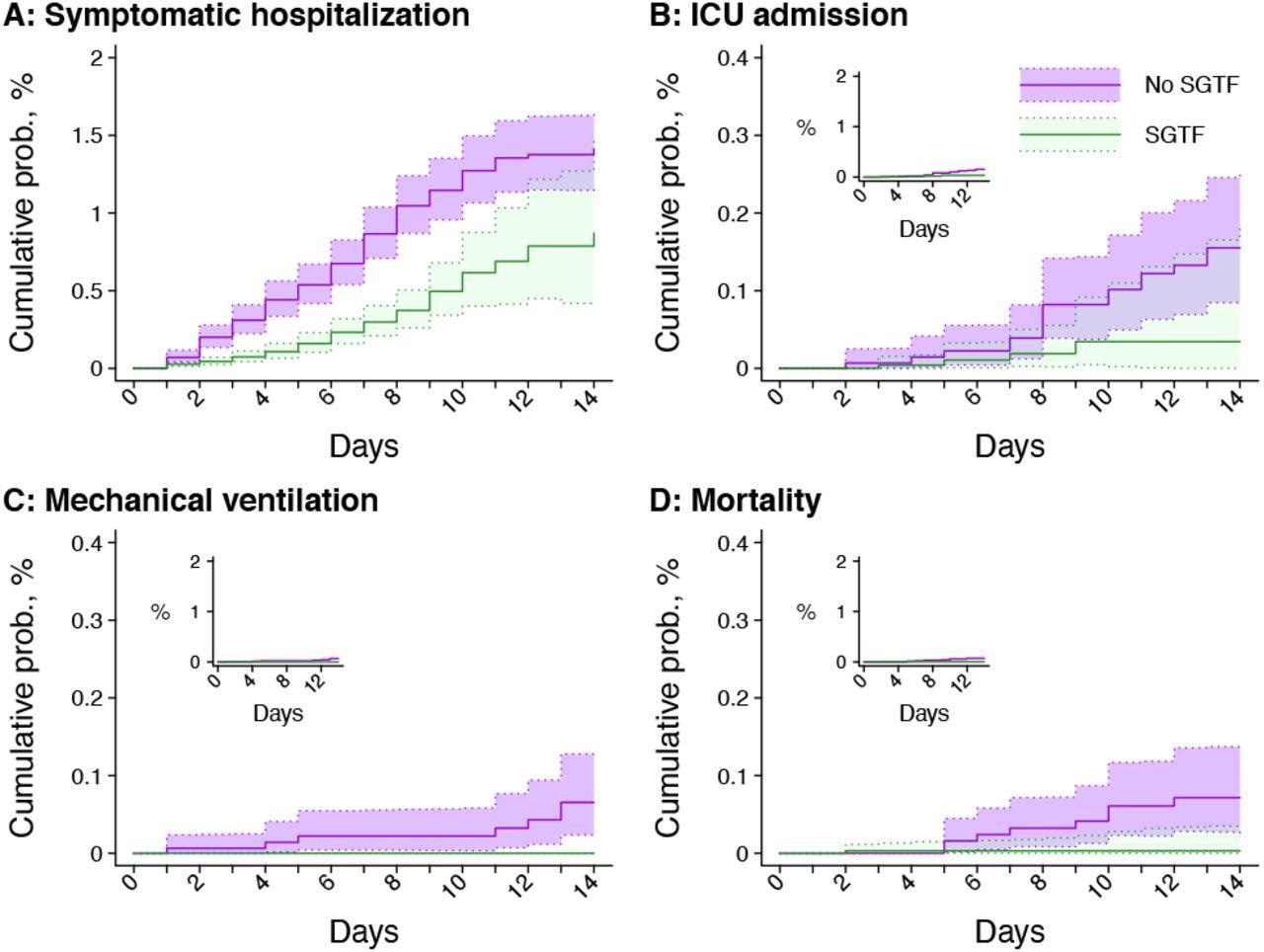
Times to severe outcomes among cases with SGTF and non-SGTF infections first detected in outpatient settings. Panels include (A) symptomatic hospital admissions; (B) ICU admissions; (C) initiations of mechanical ventilation; and (D) mortality. Inset plots within each panel illustrate cumulative probabilities on the same y-axis scale as panel A. Shaded regions denote 95% confidence intervals. Green and violet correspond to detections with and without SGTF (interpreted as a proxy for SARS-CoV-2 Omicron variant infection), respectively.
Omicron cases showed greater rates of recovery after hospitalization than Delta
Approximately 83.5% of hospitalizations for Omicron cases were complete by January 1, 2022, compared to 77.8% of hospitalizations for Delta.
All patients hospitalized for an Omicron infection were discharged to home or home-based care. Only 92.9% of Delta cases were discharged from the hospital.
People with Omicron infections had nearly 70% shorter hospital stays than Delta infections. The average hospital stay for symptomatic Omicron infections was 1.5 days and 90% of patients were expected to recover within 3 days.
The average hospital stay for Delta infections was almost 5 days.
Study limitations
There was limited time for researchers to follow up on all COVID-19 cases and their rate of hospital discharge. Data on discharge was available for 84% of Omicron cases and for 78% of Delta cases. Additionally, follow-up data for Omicron infections were shorter since they occurred towards the end of the study period.
Because there is a possibility that COVID-19 testing among the Kaiser Permanente Southern California healthcare system is different than testing in the general population, the rate of Omicron versus non-Omicron infections and hospitalizations may differ at a population level.
*Important Notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.