
With around 262 million active patients as of 2019, asthma is one of the most prevalent pulmonary diseases in the world. Though manageable with medications, it can affect the quality of life for many. Surprisingly, those suffering from the condition are seemingly less prone to brain tumors. However, how this link functions has remained unclear. Now, scientists may have finally discovered the answer.
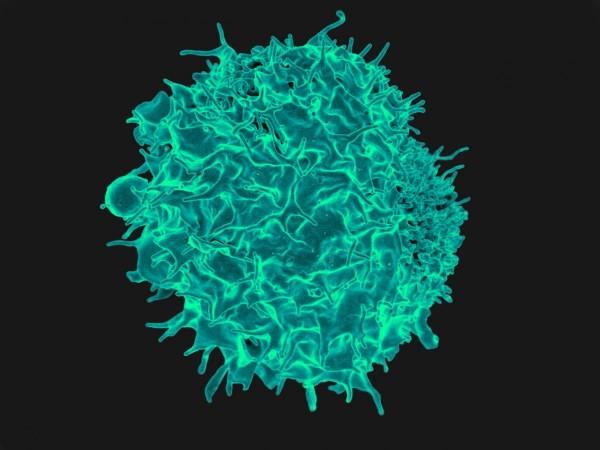
According to a new study, the action of T cells (a type of immune cell) in asthma patients could be protecting them from developing brain tumors. Using an animal model, the researchers learnt that asthma causes T cells to act in a manner that induces lung inflammation but also hinders tumor growth. It does so by secreting a protein that disrupts a pathway that promotes the growth of brain tumors. The findings were published in the journal Nature Communications.
“Of course, we’re not going to start inducing asthma in anyone; asthma can be a lethal disease. But what if we could trick the T cells into thinking they’re asthma T cells when they enter the brain, so they no longer support brain tumor formation and growth? These findings open the door to new kinds of therapies targeting T cells and their interactions with cells in the brain,” said Dr. David Gutmann, senior author of the study, in a statement.
An Unproven Association

Asthma is a long-term pulmonary disease that affects people of all ages. It causes the airways of the lungs to inflame and constrict, thereby, resulting in breathing difficulties. Several factors determine the emergence of asthma in an individual. A family history of asthma, exposure to environmental allergens and irritants, and childhood obesity, among others, play a role in triggering the onset of the disease.
A suggestion that individuals struggling with inflammatory diseases such as asthma or eczema were at a lower risk of developing brain tumors was first floated over 15 years ago. The proposal was made based on epidemiologic observations. However, there was no clear understanding as to how two highly diverse diseases could be connected. Also, scientists doubted whether a link between the two ailments did exist in the first place.
Exploring a Unique Link
Neurofibromatosis (NF) is a group of complex genetic disorders that promote the growth of tumors in the nerves, brain, and spinal cord. Children with the hereditary condition NF type 1 (NF1) may develop a form of brain tumor called optic pathway glioma. Originating from brain cells known as astrocytes, these tumors spread within the optic nerves that transmit visual information from the eye to the brain.

Around half a decade ago, Dr. Gutmann observed an inverse relationship between asthma and brain tumors among his patients. At the time, he was not certain whether a conclusive inference could be drawn from this association. However, findings from his recent studies revealed that immune cells play a vital role in the progress of optic pathway gliomas. Thus, he began exploring whether immune cells could explain the link between asthma and brain tumors.
Preventing Growth of Tumors
For the current study, the authors turned to genetically modified mice. The animals had been engineered to bear a mutation in the NF1 genes so that they developed optic pathway gliomas by the time they were three months old. Groups of mice were exposed to irritants that induced asthma [such as ovalbumin (OVA) and house dust mite (HDM)] in them between the ages of four to six weeks. For comparison, a control group was treated with phosphate-buffered saline (PBS).
The rodents were examined for optic pathway gliomas at three and six months of age. Interestingly, brain tumors were not found to grow in mice that had asthma. Through additional experiments, the team ascertained that inducing asthma in mice that were tumor-prone alters the behavior of T cells in their bodies. Once the animals developed asthma, the secretion of a protein known as decorin by T cells began.
Decorin is found in connective tissues in the human body. It is primarily synthesized by fibroblasts, smooth muscle cells, and stressed vascular endothelial cells. In asthma patients, decorin has a damaging effect. The protein interacts with tissues lining the airways of the lungs and worsens the symptoms of asthma. However, the researchers discovered that this was not the case in the brain. Decorin was found to play a beneficial role there.
In the brain, the protein acts on microglia—a subcategory of non-neuronal cells known as neuroglia that are found within the brain—and blocks their activation. It does so by interfering with the activation of the nuclear factor kappa B (NFkB) pathway, which regulates inflammatory responses. Activated microglia are known to stimulate the growth and development of cancers and tumors.
Potential to Inform Treatments
Equipped with these findings, the authors treated the mice (carrying NF1 mutations) with either decorin or caffeic acid phenethyl ester (CAPE), a compound that suppresses NFkB activation pathway. It was found to protect the tumor-susceptible mice from developing optic pathway gliomas. This suggests that the blocking of microglial activation may serve as a potential treatment approach against brain tumors.
“The most exciting part of this is that it shows that there is a normal communication between T cells in the body and the cells in the brain that support optic pathway glioma formation and growth. The next step for us is to see whether this is also true for other kinds of brain tumors,” expressed Dr. Gutmann.
The team is now evaluating the role of eczema and other early-childhood infections in the development of brain tumors as T cells are involved in both cases. Emphasizing the potential of the study in informing future treatment, Dr. Gutmann concluded: “As we understand this communication between T cells and the cells that promote brain tumors better, we’ll start finding more opportunities to develop clever therapeutics to intervene in the process.”