Do you know your risk of a heart attack? Many people are don’t know — or don’t seem to care about knowing — their risk “score”.
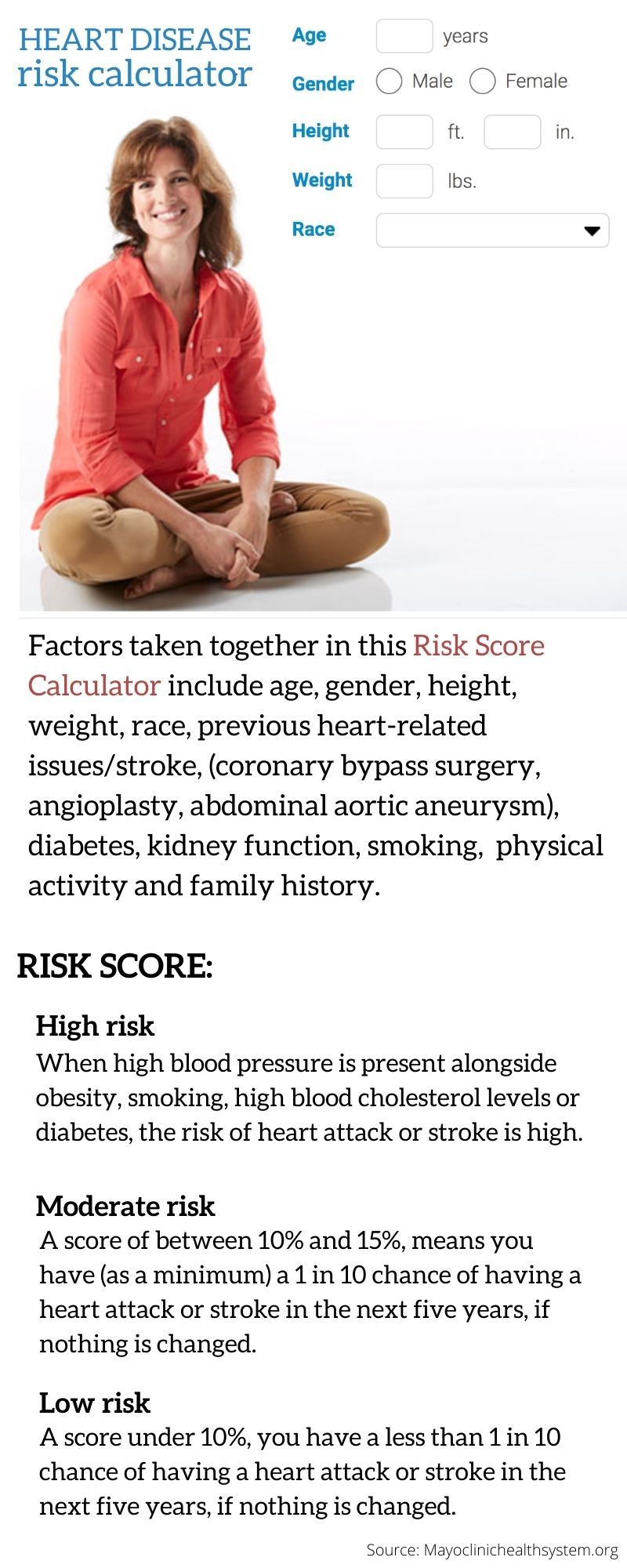
But such risk score system has been used for some time now. In general, it establishes one’s overal risk of heart disease. These tools include: cholesterol test, blood pressure, lifestyle factors (do you exercise for 150 minutes a week?), family history and others conditions such as diabetes.
But can you predict when a heart attack is likely to hit someone, with greater accuracy?
It turns out this may now be possible. A new test using artificial intelligence (AI) analysing a host of proteins in the blood has been developed promising a much higher accuracy in predicting cardiovascular “events” you may be facing.
Compared to the the existing “risk score” system, the protein-based analyser claims a 60% accuracy in predicting a risk of heart attack within a period 4 years — 48 months.
36seconds
One person dies every 36 seconds in the US from cardiovascular disease.
What’s the new test all about?
It’s known as the “protein model”. The method utilises at least 27 proteins found in the blood. This is significant: that number is about a quarter of all proteins encoded by our genes, according to experts.
Why only now?
This method has only become possible in the current age, thanks to emerging new technologies and fasting computing power, which allow experts to measure thousands of blood proteins to assess patients’ individual risk.
Who invented it?
Researchers led by Dr Stephen Williams, based in Colorado, developed the test and published their work in Science Translational Medicine journal on April 6, 2022.
Dr Williams, the chief medical officer at US-based SomaLogic, specialises in translational medicine and the development of diagnostics and management of a clinical assay laboratory. The team included 22 experts in different medical disciplines from various parts of the world to collaborate on developing the test.
LOW, MEDIUM, HIGH RISK
It uses AI to develop a predictive model. An algorithm was developed to determine the risk.
Image Credit: Seyyed de la Llata / Gulf News
How many bloods samples were used to test its accuracy?
To test the accuracy of this protein method, 32,130 “archived” plasma (amber-colored liquid in the blood) samples from 22,849 participants in nine clinical studies were used, according to the journal.
Using machine-learning, Williams’ team analysed 5,000 proteins in blood plasma samples from 22,849 people. And that’s how they identified a signature of 27 proteins that could predict the likelihood of heart attack, stroke, heart failure or death, over a period of 48 months.
What is the role of blood proteins in predicting heart attacks?
In general, heart disease (or cardiovascular risk factors) activate a number of pro-oxidative genes in the blood vessel (vascular) wall. This results in the generation of reactive oxygen species, especially those generated by the endothelium (a thin membrane that lines the inside of the heart and blood vessels).
Using modern clinical tools, measuring endothelium-dependent vasodilation (a nitric oxide-mediated process) by a variety of different techniques now provide a marker of endothelial integrity.
What is the role of the endothelium in the production of these proteins?
In medical science, it is a known fact that endothelial cells release substances that control vascular relaxation and contraction — as well as enzymes that control blood clotting, immune function and platelet (a colourless substance in the blood) adhesion.
I think this is the new frontier of personalised medicine, to be able to answer the question, does this person need enhanced treatment? And when you’ve treated someone, did it actually work?
– Dr Stephen Williams, the chief medical officer at US-based SomaLogic
These genes also incidate a complex cascade of events that underlies the transition from normal endothelial function to dysfunction. The result: abnormal heart activity, development of a pro-coagulant endothelial surface, inflammation, and, ultimately, plaque formation which progressively blocks the flow of oxygenated blood to the heart, which may eventually lead to a heart attack.
What is the significance of this new test?
Globally, heart disease is the leading cause of death — one in three — as well as disability.
In both the developed and developing world, the risk is increasing, despite the development of lipid lowering, anti-inflammatory, antithrombotic, dual antiplatelet, and anti-diabetic treatments.
A 2012 study published in the journal JAMA predicts that the risk of developing heart disease is more than 40% in mean and 30% in women over a lifetime.
–
“I think this is the new frontier of personalised medicine, to be able to answer the question, does this person need enhanced treatment? And when you’ve treated someone, did it actually work?” research leader Dr Williams said.
But can you really predict when a heart attack would strike?
According to Dr Sutter Zi-Jian Xu, a cardiologist in the Sutter Health network, people can notice subtle heart attack symptoms months before an actual event occurs.
The current risk score system — the most widely used in the world — considers a person’s age, sex, race, medical history, cholesterol and blood pressure to assess their likelihood of having a cardiovascular event.
The new 27-protein model takes this scoring method to a higher pitch.
When its predictive ability was validated against 11,609 individual cases, the researchers found their model was roughly “twice as good” as existing heart disease risk “scores”.
The new test was also able to accurately assess risk in people who have previously had a heart attack or stroke, or have additional illnesses, and are taking drugs to reduce their risk. This is where existing risk prediction scores tend to fall short.
Where does the “60% accuracy” taken from?
Overall, researchers said that in their study, less than a quarter of people testing positive had a heart attack — equivalent to a positive predictive value of 22% (at 95% confidence interval).
The test, however, accurately identified almost all patients who died or had a major cardiac adverse event within 30 days — equivalent to a sensitivity of 98.0%.

What’s the advantage of the protein test?
The most common predictor for heart attack risk is having either high LDL cholesterol (“bad” cholesterol) or low HDL cholesterol (“good” cholesterol) — or both.
In general, genetic tests can provide an idea of someone’s risk of certain diseases based on one’s genetic profile. The protein model test differs from genetic tests in that the protein analysis provides a more accurate snapshot of what someone’s organs, tissues and cells are doing at any given moment in time, William’s team explained.
HEART DISEASE FACTS:
One person dies every 36 seconds in the United States from cardiovascular disease.
About 659,000 people in the US die from heart disease each year—1 in every 4 deaths. $363 billion, annual cost of heart disease in the US, from 2016 to 2017.
[Source: CDC]
How much is this test? When can I get it?
The test is already being used in four healthcare systems within the US. The price of the test is not immediately available.
Prof Manuel Mayr, the British Heart Foundation professor of cardiovascular proteomics at King’s College London, said: “Proteins are the building blocks of our body. While this study uncovers new associations between proteins in blood and death by all causes, more research is needed to assess the potential clinical impact of using these 27 proteins, compared to current risk prediction tools for cardiovascular disease.”