
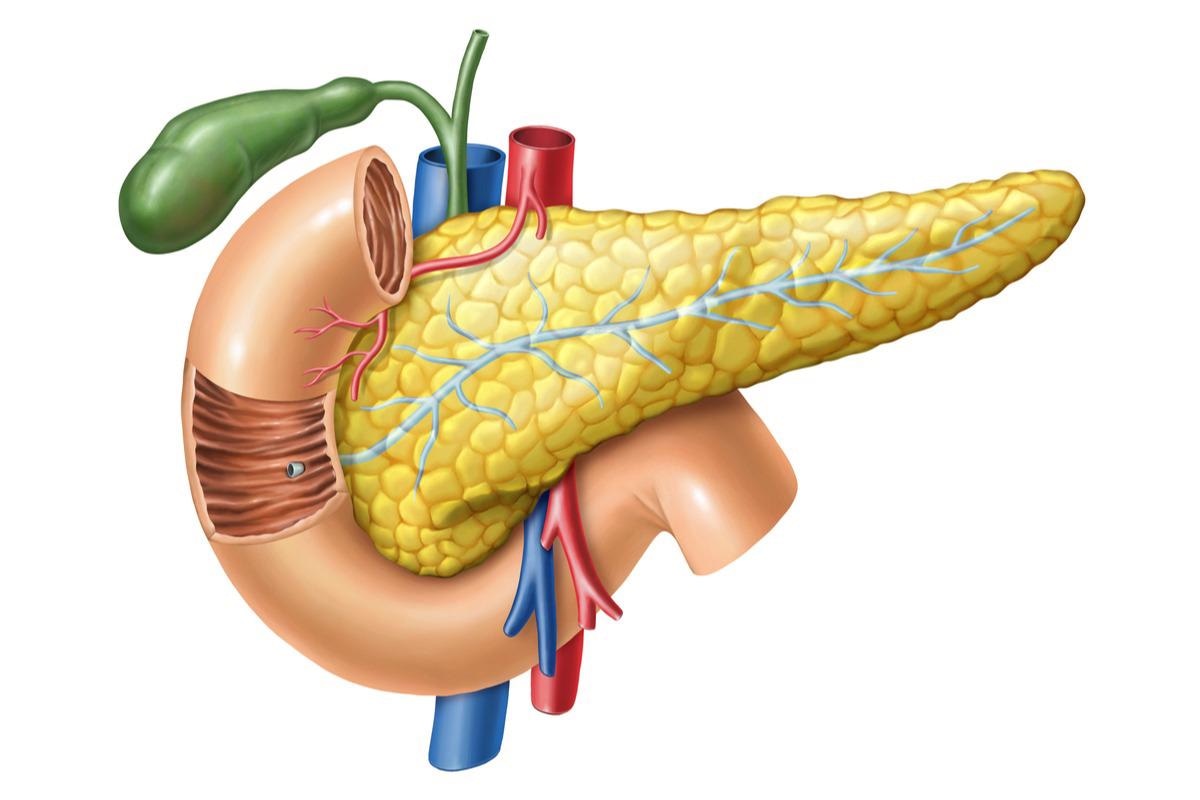
A recent study published in the journal Cell Reports investigated the impact of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection on the human pancreas.
Several studies suggest a bidirectional relationship between diabetes and coronavirus disease 2019 (COVID-19). However, other reports indicate that diabetes and hyperglycemia can increase the chances of COVID-19 infection. An in-depth evaluation of the evidence at hand is essential to understand the impact of the virus on the human pancreas and the onset of diabetes in infected patients.
About the study
The present study analyzed the consequences of COVID-19 infection on pancreatic cells and the potential of diabetes onset in an infected patient.
Samples of human pancreatic islets were collected from non-diabetic cadaveric donors through Prodo Laboratories Inc., CA. The samples were rested in Prodo islet media (Transport) (PMI(T)) before transferring them to a standard culture medium containing D-glucose, 1% penicillin-streptomycin, and 10% fetal bovine serum (FBS). The samples were then propagated on Vero E6 cell lines.
The impact of glucose on the islets was assessed with respect to the regulation of angiotensin-converting enzyme 2 (ACE2) expression and COVID-19 infection. Viral titers for Vero E6 cells infected with SARS-CoV-2 were evaluated by a plaque assay.
Human coronavirus OC43 (HCoV-OC43) cultures on an HCT-8 cell line and HCoV-NL63 stocks on an LLC-MK2 cell line were used to obtain tissue culture infectious dose (TCID50) titers for the respective cell line.
Primary human islets were infected in vitro in the absence (mock infection) or the presence of SARS-CoV-2, HCoV-OC43, and HCoV-NL63, and the tissue culture supernatant (TCS) was subsequently collected.
Results
When the pancreatic islets were treated with the recombinant SARS-CoV-2 spike (S) protein, the death of beta cells was observed. Approximately 2.5% of the islet cells were infected with SARS-CoV-2 among which insulin (INS)-secreting beta cells were more targeted as compared to the glucagon (GCG)-secreting alpha cells while cells other than alpha and beta cells showed intermediate levels of infection.
The presence of inflammation-associated proteins in the TCS containing high SARS-CoV-2 titers indicated a controlled inflammatory response involving C-X-C motif chemokine ligand 10 (CXCL10) and CXCL11 with insignificant levels of interferon-gamma (IFNƔ). SARS-CoV-2 nucleoprotein (NP) was found to be decreased in dead beta cells while no notable differences were found in the cases of live or dead alpha cells or other cells. Notably, the viral infection showed a remarkable reduction in insulin content in infected beta cells.
The onset of SARS-CoV-2 symptoms depends on the expression of various proviral host factors like the SARS-CoV-2 entry receptor ACE2. The study found ACE2 on approximately 5% of live alpha, beta, and other cells and a relative increase of the ACE2 antibody AF933 bound to early only apoptotic beta cells, and not to alpha or other cells. In contrast, late apoptotic and necrotic cells responded to the presence of AF933.
The analysis of the Vero-E6 cells infected with SARS-CoV-2 showed that the blockade of the infection caused by ACE2 protected alpha, beta, and other cells from SARS-CoV-2 infection. An infection inhibition of 96% for beta and 94% for other cells was observed for viral NP detection while ACE2 blockade effectively reduced viral titers by 99.6%.
No significant differences in glucose concentrations were observed either in the cellular viral burden, inflammatory response parameters, or infectious SARS-CoV-2 titers. SARS-CoV-2-infected islet cells had a lesser number of host-derived transcript unique molecular identifiers (UMIs) per cell, 75% of viral genes-derived total sampled transcripts, and fewer host genes detected per cell. Also, the team noted a decrease in the prediction scores of cell type label transfer for infected cells.
Conclusion
The study findings showed that SARS-CoV-2 caused a productive yet restricted infection of pancreatic islet cells and an insignificant inflammatory response. A muted impact of this extent led the researchers to negate any diabetogenic ability assigned to SARS-CoV-2 infection. Translational alterations related to COVID-19 were restricted to infected islet cell subsets and reduced several alpha cell antigens. However, COVID-19 infection can result in microvascular thrombosis which can cause diabetes in high-risk individuals.
Incorporating new epidemiological studies, expansion of histopathological investigations, and the development of new animal models are essential to resolve debates arising as a result of conflicting studies about the impact of COVID-19 infection.