This week the government announced additional vaccine booster jabs for the over-75s and suggested a further shot is likely to be needed in the autumn. But imagine if the next Covid vaccine jab you have were the last you would ever need. That’s a dream being actively pursued now by researchers, who feel it could be possible to make a “universal” vaccine against the Sars-CoV-2 virus that would work well not only against all existing variants but any that the virus could plausibly mutate into in the future.
Some are thinking even bigger. In January, Joe Biden’s chief medical adviser, Anthony Fauci, and two other experts called for more research into “universal coronavirus vaccines” that would work not only against Sars-CoV-2 but against the many other coronaviruses in animal populations that have the potential to spill over into humans and cause future pandemics. “We need a research approach that can characterise the global ‘coronaviral universe’ in multiple species,” Fauci and colleagues wrote in the New England Journal of Medicine, “and apply this information in developing broadly protective ‘universal’ vaccines against all [coronaviruses].”
Is that just a fantasy? Not necessarily. After all, many considered it fanciful, when the pandemic began, that we’d have a vaccine against Covid-19 in less than a year. But experience has proved that “we as a research community can pull together and do remarkable things,” says Larry Corey, a virologist and vaccine expert at the University of Washington in Seattle.
The current vaccines were developed against the original “ancestral” variant of Sars-CoV-2. They still work remarkably well against the new variants in preventing severe disease – Corey says that even against Delta there seems to be about a 90-fold difference in the death rate between vaccinated and unvaccinated individuals. But the Omicron variant has caused alarm by its ability to transmit faster than the others and to infect vaccinated people. Although very few such individuals develop serious symptoms from Omicron, it can actively suppress the immune defences that vaccination (as well as natural infection) activate.
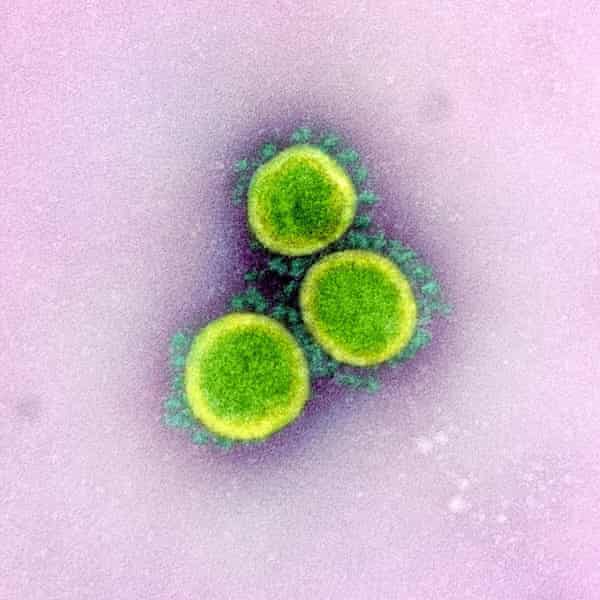
Variants acquire changes to the chemical structure of the viral proteins, through random mutations when the virus replicates, that give them some competitive advantage – improved transmissibility, say. Many of these changes happen on the so-called spike protein, which sticks out of the virus shell and latches on to proteins in the membranes of human cells, creating a point of attachment and attack. Omicron has an alarming number of such mutations, showing how much capacity Sars-CoV-2 has to spring surprises.
One answer is to adapt the vaccines to the variants. The mRNA vaccines made by Pfizer/BioNTech and Moderna contain RNA molecules that act as templates for our cells to make harmless fragments of the spike protein. This is the vaccine’s antigen, provoking the immune system to find antibody molecules that will recognise the viral protein and mobilise immune cells against it. Then if the actual virus gets into our bodies, our immune system is primed to identify and destroy it. Other vaccines, such as AstraZeneca’s, use other methods to elicit the same immune priming. If the spike protein of a variant has a slightly different structure, in principle we can change the RNA molecule to one that encodes part of this new protein.
If, as widely expected, Sars-CoV-2 eventually becomes endemic in the population, constantly circulating at a low level like flu and cold viruses but with the potential to produce an epidemic outbreak, the vaccines could be tailored to whatever variants are currently in circulation. This is more or less what happens with flu: each season’s flu vaccine is based on a best guess of what that season’s strains are likely to be.
That’s all very well – except that Omicron has shown how rapidly a significantly new variant of the coronavirus can appear and spread globally. Pfizer and Moderna are now working on a vaccine tailored to Omicron. But even if this can be made and tested within a few months, that may be too late. So a universal vaccine that can protect against all variants could be preferable. “We need a vaccine that has potential to protect broadly and proactively against multiple coronavirus species and strains,” says Kayvon Modjarrad, who leads a team seeking to develop one at the Walter Reed Army Institute of Research in Silver Spring, Maryland.
At the moment we have no pan-variant vaccine for any endemic virus. Researchers have long dreamed of a universal vaccine that would make flu epidemics less lethal, and there are now promising signs that it could be possible. The design principle for a universal Covid vaccine would follow similar lines.
One option might be to prime the immune system to recognise not just one bit of a viral protein, but lots of bits – not all of which are likely to change (or change significantly) at once in any new variant. We’d give the immune system many different ways to spot, and then suppress, the invader, in the hope that one will work. This might involve, for example, making an mRNA vaccine that contains many different RNA molecules, each encoding as a different protein fragment. Or a single particle in the vaccine could hold several different fragments.
Alternatively, you can look for parts of the virus that seem to be “conserved” across variants: proteins (or bits of them) that don’t mutate much at all, presumably because such changes would be too detrimental to the virus. But how can you know what those will be, even for variants that haven’t emerged yet? One way is to see if highly conserved protein regions exist already among a whole family of related coronaviruses. “If you can find things that are in common between Sars-CoV-2, Sars [the related respiratory virus that caused alarm in 2003], and a bunch of other animal coronaviruses, then the likelihood is that the next variant of Sars-CoV-2 will have them too,” says Skip Virgin, chief scientific officer of San Francisco-based Vir Biotechnologies, which is working with GlaxoSmithKline on vaccine development – a collaboration that has already produced the monoclonal antibody sotrovimab for alleviating Covid symptoms.
At the moment, researchers are mostly striving for the relatively modest target of hitting just a subset of the coronavirus universe: typically, to stimulate an immune response against a part of the spike protein, called the receptor binding domain (RBD), shared by Sars, Sars-CoV-2 and closely related bat coronaviruses. The RBD is the part of the spike protein that latches on to the host cells. Although some of the variants have small mutations in their RBD, its chemical structure doesn’t change much: create a strong immune response to the RBD and it should work against any virus in this family.
Modjarrad’s team began Phase I clinical trials (looking just at the safety) of their pan-variant vaccine in April 2021. It uses a tiny nanoparticle called ferritin – a natural protein that stores iron atoms in the body – studded with many copies of the Sars-CoV-2 RBD.
It has been long known that many copies of an antigen in a single vaccine particle elicit a stronger immune response than a single copy does. The institute is cagey about releasing details of its progress until its clinical trial data has been published. In December, however, the team published results showing that their ferritin vaccine confers good protection in macaques not only against the ancestral form of Sars-CoV-2 but also against the Alpha, Beta, Gamma and Delta variants, and the original Sars virus.
Barton Haynes of the Duke University School of Medicine in North Carolina is taking a similar approach with RBD-studded ferritin-based nanoparticles. Last May he and his coworkers reported a candidate vaccine that protected macaques against Sars-CoV-2, Sars, and some Sars-like bat coronaviruses. Very recently they showed that it generates a good immune response against the Delta and Omicron variants too.
Haynes says they hope to start human clinical trials at the end of 2022. If they work out, he thinks that it might take a year or two before the vaccine is ready to use, depending on whether it’s deemed different enough from those we have already to warrant another large-scale Phase III clinical trial before being approved.
These efforts might yield a vaccine resistant to all SARS-CoV-2 variants – but in principle such approaches might have an even wider scope, offering the universal coronavirus vaccines that Fauci and colleagues have called for. Haynes says that would probably entail finding the crucial RBDs for other families and adding those on to the particles too. That’s the beauty of the nanoparticle approach: it can readily incorporate a variety of protein fragments into a so-called multivalent vaccine.
Finding the right protein fragments could mean combing through the thousands of coronaviruses known to infect wild animals such as bats, civet cats and raccoon dogs, as well as the four coronaviruses already endemic in human populations and which cause mild cold-like respiratory symptoms. It would be a huge task. But now we know the awful dangers such coronaviruses (which include those that caused outbreaks of Sars in 2003 and Mers in 2012) pose, the investment would be cheap compared with the economic and social harm it might prevent. Haynes hopes it might ultimately be possible for a single jab to protect against all coronaviruses for five to 10 years.
Of course, no one can be sure what the fiendishly ingenious Covid-19 virus has in store for the future. “The first axiom of infectious disease is, never underestimate your pathogen,” says Corey. “The rapidity with which we’ve got four major variants in two and a half years is unprecedented and surprising. One wouldn’t bet against this virus.”
But even viruses have limits. For example, despite Omicron’s extensive set of mutations, Vir’s sotrovimab still works against it. “Viruses can change some things but have a really hard time changing others,” says Virgin. “There are some things a virus just can’t get away with changing.” If you can find them, you’re in business. “I am optimistic that we can generate a vaccine that will give truly broad protection,” he says.
Even the current vaccines still do well at preventing deaths, and we’re building up an arsenal of antivirals and other treatments too. What might be more important now, Corey says, is a vaccine that does better against all variants at blocking transmission. Even when death rates are reduced, “we are seeing the fabric of our lives, our travel, the things that make modern culture, be interfered with enormously,” he says. So we need second-generation vaccines that can prevent widespread infection – a goal that Corey says is widely regarded as tougher, and which would be hard to assess until they are rolled out.
It’s tempting to think that we need to solve this pandemic before preparing for the next one, says Virgin, but “there’s absolutely no reason that your pandemic response can’t prepare you for the next”. And after all, he adds, it’s easier to persuade governments to spend on solving an existing problem than on one that hasn’t happened yet.
“We really want to get to the point where we’re preventing the next pandemic, not responding to it,” says Neil King of the University of Washington in Seattle, who is also developing a universal nanoparticle-based coronavirus vaccine. “The only way to do that is through broadly protective vaccines.” How marvellous it would be if, in developing a variant-proof Covid vaccine, we end up with one that can avoid the next pandemic too.